Online Report
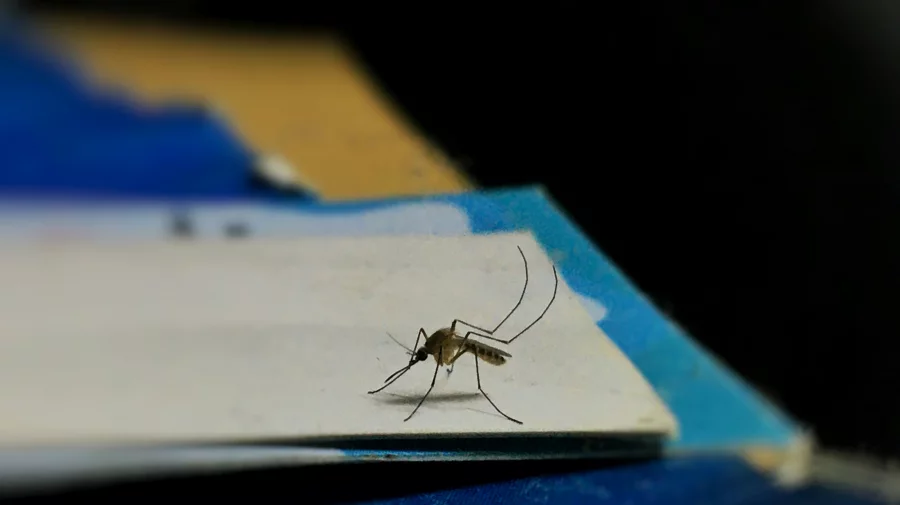
Mosquitoes are among the deadliest creatures on Earth, killing more human lives than any other animal. Mosquitoes kill about 750,000 people every year, placing them at the top of the list, while humans are second, causing 437,000 deaths annually.
The World Health Organization has already issued a warning that due to climate change, half of the world’s population is now at risk of dengue, with Bangladesh being no exception. According to the Disease Control Unit of the Directorate General of Health Services, nearly 9,500 patients have been hospitalized with dengue this year. Against this backdrop, the world observes World Mosquito Day on August 20, which has been there since 1930.
Mosquito-borne diseases have been recorded in human history for thousands of years as a leading cause of illness and death. Until the late 19th century, no one understood that mosquitoes were disease vectors. The first breakthrough came in 1877, when British doctor Patrick Manson discovered that a species of Culex mosquito could transmit the filarial worm to humans.
Over the next two decades, he and other researchers from France, Italy, Russia, and the United States focused on malaria, a major killer in tropical and temperate countries. Gradually, they began to understand the complex connection between humans, mosquitoes, and malaria transmission.
In 1894, Manson and Ronald Ross, a medical officer in the Indian Medical Service, began researching mosquitoes as possible vectors for the malaria parasite. After years of tireless work, in 1897 they proved that Anopheles mosquitoes could carry the malaria parasite. They named the day of their discovery; August 20, 1897 — “Mosquito Day.” Later, the London School of Hygiene & Tropical Medicine renamed it “World Mosquito Day” to preserve the significance of the finding, and it is now observed annually.
In the context of Bangladesh, this day is highly significant. As a warm and humid country, Bangladesh’s climate is ideal for mosquito breeding. The high density and diversity of mosquito species mean a greater risk of mosquito-borne diseases. According to research, 126 species of mosquitoes have been identified in Bangladesh, of which 14–16 species are usually found in Dhaka. Major mosquito-borne diseases in Bangladesh include dengue, chikungunya, malaria, filariasis, and Japanese encephalitis.
The first recorded appearance of dengue in Dhaka was in 1963, when it was known as “Dhaka Fever.” The first major outbreak occurred in 2000, when scientists identified it as dengue. That year, 5,551 people were infected, and 93 died.
Since then, dengue has occurred almost every year to varying degrees, but in 2019 it reached epidemic proportions, with 101,354 hospital admissions and 179 deaths. While cases dropped somewhat during the Covid-19 years, 2023 saw the highest number in Bangladesh’s history, with 321,179 cases and 1,705 deaths. In 2024; 101,214 people had been hospitalized with dengue, and 575 had died.
By this year, 2025, nearly 27,000 dengue cases and over 100 deaths have been reported. In reality, the true number of infections may be five times higher, as many people with mild symptoms do not seek hospital care, making it harder to fully grasp the scope of the problem.
Chikungunya, a disease similar to dengue, was first detected in Bangladesh in 2008. It is spread by Aedes mosquitoes. From 2011 to 2017, cases were recorded almost every year, with the largest outbreaks in Dhaka occurring in 2016–2017.
Newspaper reports indicate that in Chittagong, an average of 75% of patients with fever at private hospitals and diagnostic centers have tested positive for chikungunya, evidence of its alarming spread. Due to the foremost focus on dengue, chikungunya is not being tested widely, and many hospitals lack testing kits. It is essential to prioritize detection of this disease alongside dengue.
Malaria is another major mosquito-borne disease in Bangladesh, transmitted by seven Anopheles species. It is prevalent in nearly 72 upazilas across 13 districts, mainly in the hill tracts and border areas. Bangladesh’s malaria control history has seen ups and downs; DDT was effective during the Pakistan era, but its post-independence ban led to a resurgence.
Since the government declared malaria a national public health problem in 1990, conditions have improved. Cases dropped from 84,690 with 154 deaths in 2008 to 13,099 cases and 6 deaths in 2024. This success is due to integrated government-NGO efforts, free distribution of long-lasting insecticide-treated nets, rapid diagnostic testing, ACT treatment, and community health worker training, with support from WHO, the Global Fund, and BRAC.
However, challenges remain, especially in remote hill areas like Bandarban, Rangamati, and Cox’s Bazar, where prevalence is still high. Cross-border transmission from India and Myanmar, climate change effects, and drug-resistant malaria strains pose ongoing threats. Limited health facilities and low awareness among indigenous communities further complicate eradication efforts.
Filariasis (locally known as elephantiasis) is another debilitating mosquito-borne disease in Bangladesh, causing abnormal swelling of limbs and other body parts. Once widespread, it has been brought under control through the government’s Filariasis Elimination Program. It is caused by Wuchereria bancrofti worms, transmitted by Culex and Mansonia mosquitoes.
Japanese encephalitis, also spread by Culex mosquitoes, was first detected in Bangladesh in 1977 in the Madhupur forest area. Since then, cases have been reported sporadically in Rajshahi, Rangpur, Chittagong, and Khulna regions, though little recent research means the current burden is unclear.
I began researching dengue in 2000 when it was first identified here, and for 26 years I have worked on mosquitoes both in the lab and the field, covering every corner of Dhaka and traveling to outbreak areas across the country. My team has studied nearly every type of insecticide used for mosquito control worldwide and found that some used in Bangladesh are ineffective.
Through over a hundred articles, I have detailed scientific, integrated mosquito management proposals. In 2019, a judicial committee investigated lapses in mosquito control, where I served as an expert. That same year, mosquito control at Dhaka Airport went to court, and I presented my control model to the High Court, both orally and in writing.
On February 5, 2024, the court issued a ruling calling for the establishment of a dedicated mosquito and vector-borne disease research institution, to be named the Vector Control Research Centre (VCRC). Unfortunately, despite the urgency, no steps have been taken to establish it.
Mosquito control is primarily the responsibility of local government bodies; city corporations, municipalities, district, upazila, and union councils. These organizations need trained mosquito control personnel and entomologists. While city corporations have posts for entomologists, they remain vacant for unknown reasons, despite repeated recommendations to fill them.
With dengue season upon us, we must act now. To save lives, prevent public suffering, and avoid economic losses, Bangladesh needs a sustainable, well-implemented plan.
Like other countries, we require a national institution for research and control of mosquito-borne diseases. Coordinated action between the local government ministry, health ministry, entomologists, researchers, and other stakeholders can protect Bangladesh from these deadly threats.
Professor Dr Kabirul Bashar is an Entomologist & Public Health Specialist, Department of Zoology, Jahangirnagar University. s